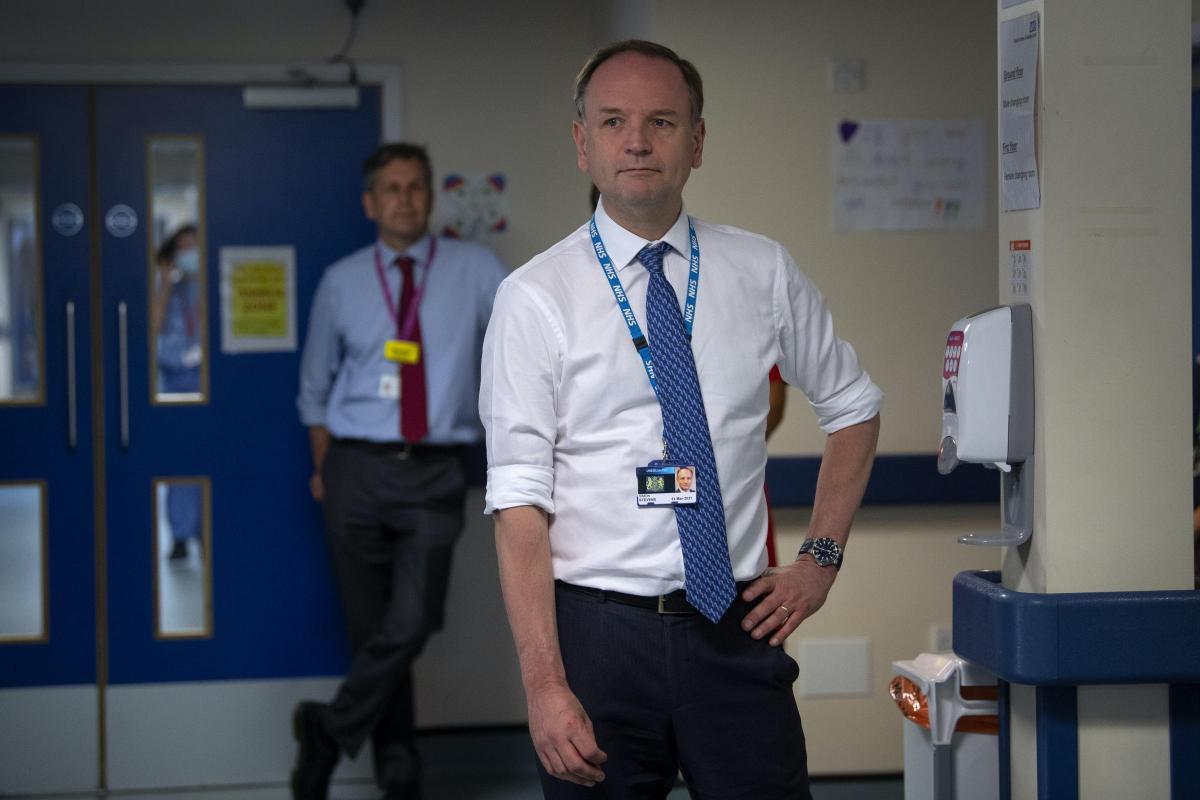
The number of elective hospital appointments dropped to around a quarter of usual levels at the start of lockdown, with the highest drop of more than half a million seen in April alone, the chief executive of NHS England has said.
The backlog of appointments will go down before increasing significantly in the latter half of the year as more people are expected to be referred, the Health and Social Care Committee heard on Tuesday.
When asked how many appointments were cancelled in England due to the crisis, Sir Simon Stevens told the virtual meeting: “The number of elective admissions in March and April was around 725,000 lower than what we might have expected given pre-Covid levels of growth.
“The drop was greatest in April when there were around 530,000 fewer elective episodes. That number has begun to recover quite significantly since then.”
Simon Stevens says the NHS had 725,000 fewer hospital admissions in March and April based on pre-COVID levels, with the greatest drop in April, but that number has begun to recover to around 55% of pre-Covid levels and going into July and August we are on track for it to be 75%
— Health and Social Care Committee (@CommonsHealth) June 30, 2020
He said at its worst, it fell to a quarter of the usual level around the March-April period, which has “rebounded to around 55-60%” and is going up.
He added: “Such that we think we may be at around three quarters of usual activity going into July-August on the elective activity.”
Sir Simon said cancer care, including surgery, continued at a much higher level in the March-April period.
He added: “Although there was a drop-off in referrals we saw around 96% of the usual treatment starts for cancer over that period.
“Paradoxically, the waiting list will go down before it goes up, potentially significantly.
“The reason for that being that fewer people are coming forward and being referred onto a waiting list.
“We’ve seen the overall waiting list drop by over half a million people between February and April, but we expect that as referrals return that will go up over the second half of the year.”
Meanwhile, Sir Simon said there was a “big unknown” over how much extra pressure has been added to the NHS for mental health care as a result of the pandemic.
He said the extra capital funding announced by the Prime Minister on Tuesday, of which £1.5 billion will be going to hospitals, will help NHS providers to phase out outdated mental health “dormitory wards”.
He told the committee: “There is a big unknown as to how much of additional burden of mental ill health there will be coming out of the last four months.”
He added: “I think in a nutshell we believe there will be an increased mental health demand but the precise size and shape of it is yet to be determined and seen.”
He continued: “One of the things we also know is that too many of the buildings and facilities in which NHS mental health care is being delivered are out of date and need a significant upgrade.
“And that’s why one of the things I have been personally pushing, and really pleased that the Prime Minister’s announcement today (Tuesday) gives effect to, is capital investment to phase out altogether so-called mental health dormitory wards.”
To deal with the potential increase in referral rates, Sir Simon said the NHS would take a “Nightingale approach” to new dedicated diagnostic facilities.
He said the first of those would be the Exeter Nightingale Hospital which will be re-purposed for non-Covid CT scanning from Monday.
He said: “It’s worth remembering that four-fifths of the patients who are on a waiting list are typically waiting for a test or an outpatient appointment, rather than waiting to be admitted to hospital for an operation.
“And given the pressures on hospitals and diagnostic teams over the March, April, May period, there has been a big reduction in the flow of patients through those diagnostic services.
“Therefore, we’ve got to do something different, we’ve got to expand diagnostic capacity, we’ve also got to do it in new ways.”
Sir Simon said that A&E admissions from March to May were about a third lower than what might have been expected, namely about 530,000 cases lower.
He said there is now a “significant rebound” in A&E attendances, which are back to about two-thirds of their normal levels, and emergency admissions which are now at about 85% of their normal level.
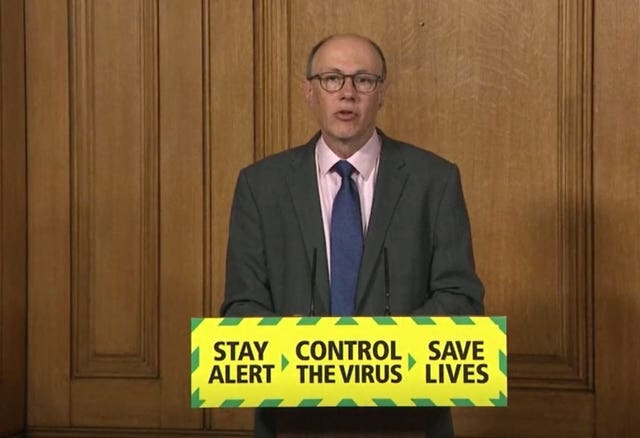
Professor Stephen Powis, national medical director at NHS England, said plans are being drawn up to try and deal with crowded A&Es, particularly in light of the pandemic where keeping patients and staff safe along with a need for social distancing are important.
Prof Powis said that ensuring the 111 call service is used prior to people showing up at the A&E departments could help direct them the to the most appropriate treatment.
He said: “We are piloting various forms of that call-first (system) in London, Portsmouth and other areas too because we want to make sure that we get the exact model right.”



Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel